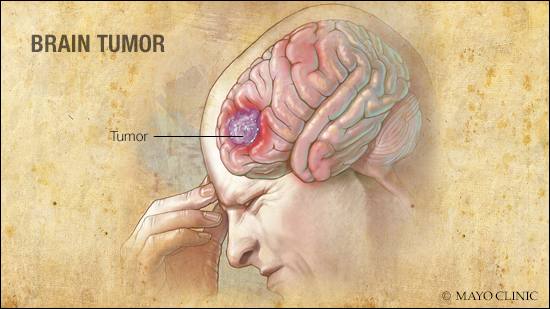
DEAR MAYO CLINIC: I have been diagnosed with a brain tumor and advised to have radiation therapy. I’m very nervous about this and the risks for me, my family and, potentially, another cancer diagnosis. Can you explain why radiation therapy could be right for me?
ANSWER: Radiation therapy has been used to treat cancer since the beginning of the 20th century. This type of treatment continues to be one of the most effective treatments for cancerous (malignant) and noncancerous (benign) brain tumors. How it is delivered — and the technology used — has continued to evolve and improve.
Most patients with brain tumors receive one of two types of radiation: external beam radiation, in which the tumor is treated over the course of several weeks, or radiosurgery, in which patients receive a high dose of radiation in one to five treatments to destroy the tumor.
Stereotactic radiosurgery uses 3D imaging to target high doses of radiation to the tumor with minimal impact on surrounding healthy tissue. It is used in small cancerous and noncancerous tumors and can be delivered in a few ways:
- Gamma Knife: A Gamma Knife is not a knife at all but rather many tiny beams of radiation focused on a tumor with extreme accuracy.
- Linear accelerator: A linear accelerator aims high-energy beams to a precise point on the body.
- Proton beam: Using positively charged particles in atoms, proton therapy is focused on the tumor; virtually none of the radiation exits beyond the tumor.
Radiosurgery targets each tumor individually and helps to spare normal tissue from being treated with radiation.
When I speak to patients, I often highlight several advantages of radiation therapy:
Radiation treatment plans are tailored to each patient.
Radiation therapy is not one-size-fits-all. The volume, dose, type and duration of radiation are tailored to fit each person and their specific tumor. A treatment plan is designed that considers the size, location and type of your brain tumor. Radiation therapy can be used to treat brain tumors by itself or after surgery, to ensure that leftover cancer cells are destroyed.
Better precision.
Radiation therapy must be accurately delivered to successfully destroy the tumor and prevent the tumor from coming back. Improvements made over the years — including improved imaging to better target the tumor and align the patient during radiation treatment — allow us to minimize damage to surrounding tissues and organs. Today, the accuracy with which we can deliver the treatment is within millimeters, thus limiting excess exposure of healthy tissues to radiation.
Better precision has allowed for a newer approach in radiation therapy, known as hypofractionated stereotactic radiotherapy, which delivers high doses of radiation over two to five days to destroy the tumor.
For instance, larger brain tumors have been difficult to treat with radiosurgery as the risk of treatment increases with the size of the tumor. However, research has shown that if we spread that dose over two to five days instead of one day, the tolerance is better, and we can often achieve a more effective dose for larger tumors.
Though side effects from brain radiation vary, fatigue and hair loss are the most reported. However, most patients find they can continue their regular activities throughout treatment.
Improved safety.
A common misconception when patients hear the word radiation is that radiation will cause cancer. While that is possible, the risk of developing a second cancer from radiation is extremely low. Modern radiation therapy techniques have improved effectiveness and safety, and radiation oncologists continue to discover ways to limit exposure and reduce the risk of secondary cancers from radiation.
It is important to note that if a secondary cancer were to occur from radiation therapy, it would not likely develop until many years after radiation exposure. Also, the risk of developing secondary cancer decreases with time, according to the American Cancer Society.
Another misconception is that radiation therapy can pose a risk to people around you. External beam radiation passes right through the body like an X-ray. Patients do not leave their treatments radioactive. You will not expose anyone to radiation by receiving this type of treatment.
Radiation therapy continues to evolve through research conducted by Mayo Clinic and others. In addition to advances in machinery, imaging has improved to help guide more accurate radiation treatment for patients.— Jennifer Peterson, M.D., Radiation Oncology, Mayo Clinic, Jacksonville, Florida