Melissa Neuman dreaded getting mammograms. Her small, dense breasts made the screening exceptionally uncomfortable and painful. So Melissa put off getting an annual mammogram until she felt she couldn’t delay any longer.
For about five years, Melissa had been plagued with a nagging pain just under her left breast. In February 2023, a recommendation from a friend led her to seek care from Jessica Johnson, an OB-GYN nurse practitioner with Mayo Clinic Health System in Owatonna, Minnesota.
She took me seriously, was curious and determined to find out what was causing the pain,” says Melissa, who lives in Owatonna and works as an activities assistant at a local assisted living and memory care facility.
During their appointment, Jessica noticed that Melissa hadn’t had a mammogram for several years. When Melissa explained why she was reluctant to be screened, Johnson suggested she have a breast MRI.
“I’d still be getting screened, but with less pain,” says Melissa. “So I said, ‘Let’s do it.'”
The MRI revealed an area of concern. Jessica recommended that Melissa have a biopsy, but it would require a mammogram first. That’s when Melissa met Amanda Steinberg, a radiology technologist in Owatonna. She was just the person Melissa needed.
Overcoming mammogram fears, pain
“Mammograms aren’t a favorite activity for women,” says Amanda. “While it’s a preventive screening, we have mammograms to make sure we don’t have breast cancer. It’s scary.”
At 35, Amanda had her own scare with a mammogram that showed an area of concern, so she understands her patients’ fears and reluctance. She strives to set them at ease, explain simply and clearly what she’s doing, take their mind off the compression and be as quick and effective as possible.
That understanding and empathy resonated with Melissa. So did Amanda’s technique. Amanda had learned that mammograms can be less painful if the patient doesn’t reach forward to grip the handles on the machine.
“When you grip or make a fist, your pectoral muscles tense up. Squeezing a muscle that is already tight makes the pinching feeling of compression feel worse,” she says.
That clenching also can create an undesirable “C” shape on the image. So instead, she tells patients not to raise their arms and grip but to let them hang relaxed by their sides.
“Women have told me how much better it is,” says Amanda.
Melissa agrees. “She was amazing, and I will never forget her, and I wish I’d found her sooner,” she says.
A closer look reveals a tumor
The mammogram and a subsequent ultrasound were inconclusive, so Johnson ordered a biopsy that was performed on Dec. 6, 2023. Two days later, Melissa learned that the biopsy had confirmed an invasive ductile carcinoma tumor positioned right up against her chest wall.
“Suddenly, everything was insane,” says Melissa.
The whirlwind of preoperative tests and appointments began, and she was informed of her options: a lumpectomy, radiation or a single or double mastectomy.
After talking through the options with her husband, Rick, she opted for a double mastectomy.
“I didn’t want to undergo MRIs every six months or worry for the rest of my life,” says Melissa.
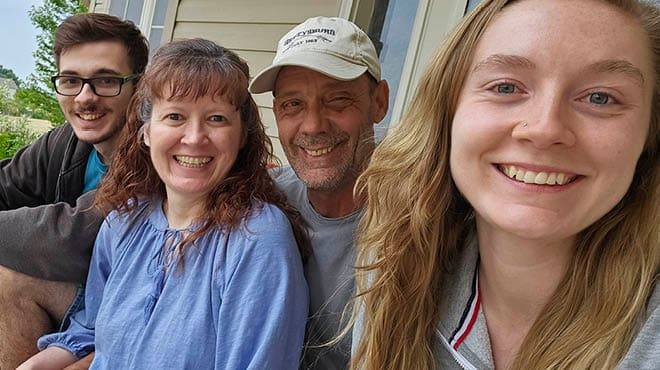
Melissa met with Mayo Clinic Health System surgeons and had a double mastectomy on Jan. 30. After one night in the hospital, she was home and recovering with help from Rick and their children, Sarah and Joshua.
Before starting her on hormone-blocking cancer medication, Melissa’s oncologist, Mina Hanna, M.D., ordered a bone density scan. Melissa was delighted to learn that Amanda would conduct it since she had such a positive experience with the mammograms.
“After I’ve done mammograms for a patient, I usually don’t know their results or even see them again,” says Amanda. “Doing Melissa’s bone density scan felt like it was meant to be that we’d be on this journey together.”
Genetics, recovery and a night at the ballpark
At the start of her breast cancer journey, Melissa was surprised to learn her diagnosis because she didn’t know of any women in her family who had breast cancer. Tests revealed the cancer was both estrogen and progesterone-positive but negative for BRCA 1 and 2 markers. Melissa wanted to learn more, so she underwent in-depth genetics testing, none of which indicated a genetic predisposition for breast cancer.
“I wanted to do extra testing so my daughter and son would have that information,” says Melissa. She’s now taking the hormone-blocking cancer medication and continuing her recovery.
“Everyone on my care team — Jessica, Amanda, Dr. Hanna, my surgeons and everyone else — has been so great,” she says.

To celebrate her progress, Melissa threw out the first pitch at Cancer Survivors Night, sponsored by Mayo Clinic Health System, at a recent Mankato MoonDogs baseball game.
“This was my first outing since my surgery, and it was so fun and inspiring. I just hoped I’d throw a good pitch,” says Melissa.
Continuing to advance, refine mammograms
Amanda is proud of her role in helping detect Melissa’s breast cancer — and that of her other patients.
“I’ve always wanted to learn and do new things with mammography,” she says.
She is particularly excited about new 3T MRI equipment in Owatonna, which will allow for MRI biopsies and more advanced imaging.
“This equipment will provide more support for breast procedures,” she says. “And more patients will be able to stay close to home for first-rate care without traveling to Mayo Clinic in Rochester.”
Melissa adds that her experience is a good example of why it’s important for doctors and others working in healthcare to take women’s health concerns seriously and provide them with options for preventive health scans and healthcare.
“If I didn’t have a provider who listened and came up with a breast MRI to screen for breast cancer, we wouldn’t have found it this early,” she says.
This article first published on the Mayo Clinic Health System blog.