ROCHESTER, Minn. — Drugs that selectively kill senescent cells may benefit otherwise healthy older women but are not a “one-size-fits-all” remedy, Mayo Clinic researchers have found. Specifically, these drugs may only benefit people with a high number of senescent cells, according to findings published today in Nature Medicine.
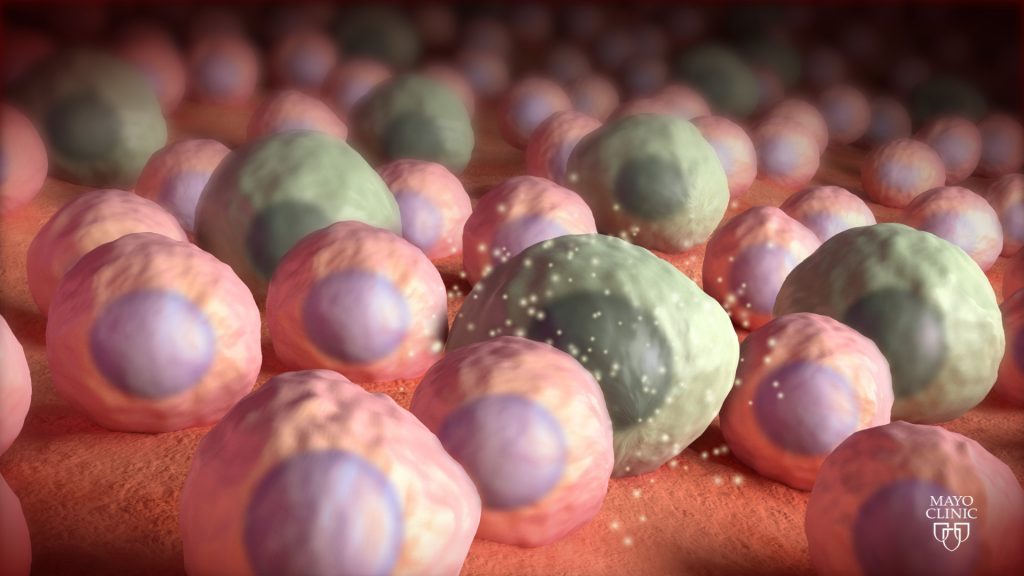
Senescent cells are malfunctioning cells in the body that lapse into a state of dormancy. These cells, also known as “zombie cells,” can’t divide but can drive chronic inflammation and tissue dysfunction linked to aging and chronic diseases. Senolytic drugs clear tissues of senescent cells.
In the 20-week, phase 2 randomized controlled trial, 60 healthy women past menopause intermittently received a senolytic combination composed of FDA-approved dasatinib and quercetin, a natural product found in some foods. It is the first randomized controlled trial of intermittent senolytic treatment in healthy aging women, and the investigators used bone metabolism as a marker for efficacy.
Researchers found that this combination, known as D+Q, had beneficial effects on bone formation but did not reduce bone resorption or the breakdown and removal of bone tissue. Furthermore, D+Q mainly benefited people with evidence of a high number of senescent cells. This group had more robust increases in bone formation, decreases in bone resorption, and an increase in bone mineral density at the wrist.

“Our findings argue against what many people are already doing — using commercial products like quercetin or related compounds like fisetin that may show some senolytic properties,” says senior author Sundeep Khosla, M.D., an endocrinologist at Mayo Clinic in Rochester, Minnesota. “They’re using them as anti-aging agents without knowing if they have high enough senescent cell numbers to benefit, or what dose or dosing regimen is needed to be effective yet safe.”
Dr. Khosla says more research is needed to better identify people who may benefit from senolytic treatments and to develop more specific and potent senolytic drugs that may show efficacy in more people. People who have experienced “accelerated aging” — such as cancer survivors after chemotherapy, or those with progeroid syndromes – may have increased numbers of senescent cells.
Besides their application to aging, senolytic drugs may be useful against certain diseases, such as idiopathic pulmonary fibrosis, dementia, diabetes, heart disease and others, Dr. Khosla says. However, these drugs will likely need to be customized according to their potency and the amounts of senescent cells in the diseased tissues.
The study was supported by National Institutes of Health grant nos. R21 AG065868, P01 AG062413, R01 AG 076515, R01 DK128552, R01 AG055529, R37 AG13925 and R33 AG61456.
Co-authors are Joshua Farr, Ph.D., Elizabeth Atkinson, Sara Achenbach, Tammie Volkman, Amanda Tweed, Stephanie Vos, Ming Ruan, Jad Sfeir, M.D., Matthew Drake, M.D., Ph.D., Dominik Saul, M.D., Madison Doolittle, Ph.D., Irina Bancos, M.D., Kai Yu, M.D., Tamara Tchkonia, Ph.D., Nathan LeBrasseur, Ph.D., James Kirkland, M.D., Ph.D., and David Monroe, Ph.D.
Drs. LeBrasseur, Tchkonia and Kirkland have financial interests related to this research, including Mayo Clinic patents and pending patents covering senolytic drugs and their uses. The remaining authors declare no competing interests.
###
About Mayo Clinic
Mayo Clinic is a nonprofit organization committed to innovation in clinical practice, education and research, and providing compassion, expertise and answers to everyone who needs healing. Visit the Mayo Clinic News Network for additional Mayo Clinic news.
Media contact: